Could Surgical Fads Have Something in
Common With the World’s Most Famous Secret Agent?
by Kari Kanto, Clare Ardern, Jonathan Scott, Simo Taimela, Trevor Corson, and Teppo Järvinen
September 10, 2024
Clinical Orthopedics and Related Research

In the early 1970s in England, a junior house officer in orthopaedics named Jonathan Scott noticed a strange pattern. His supervisor would get excited about a cutting-edge technique and splurge on boxes of new equipment. Soon afterward, Scott would notice the department’s previous “state-of-the-art” instruments gathering dust. As time went on, he witnessed other cycles of infatuation and disillusionment, including the quick rise and demise of surgery with transvaginal mesh, a device that was similarly embraced and then largely shunned.
Scott felt this pattern was troubling and ought to be called out. The question was, how to do so without making his fellow doctors feel like they were under attack? An encounter with the concept of a parabola finally gave him an idea. Scott mapped out his own parabola with tongue-in-cheek captions and sent it off to the British Medical Journal for their annual Christmas issue, where it appeared in 2001, titled “Scott’s parabola: The rise and fall of a surgical technique”.
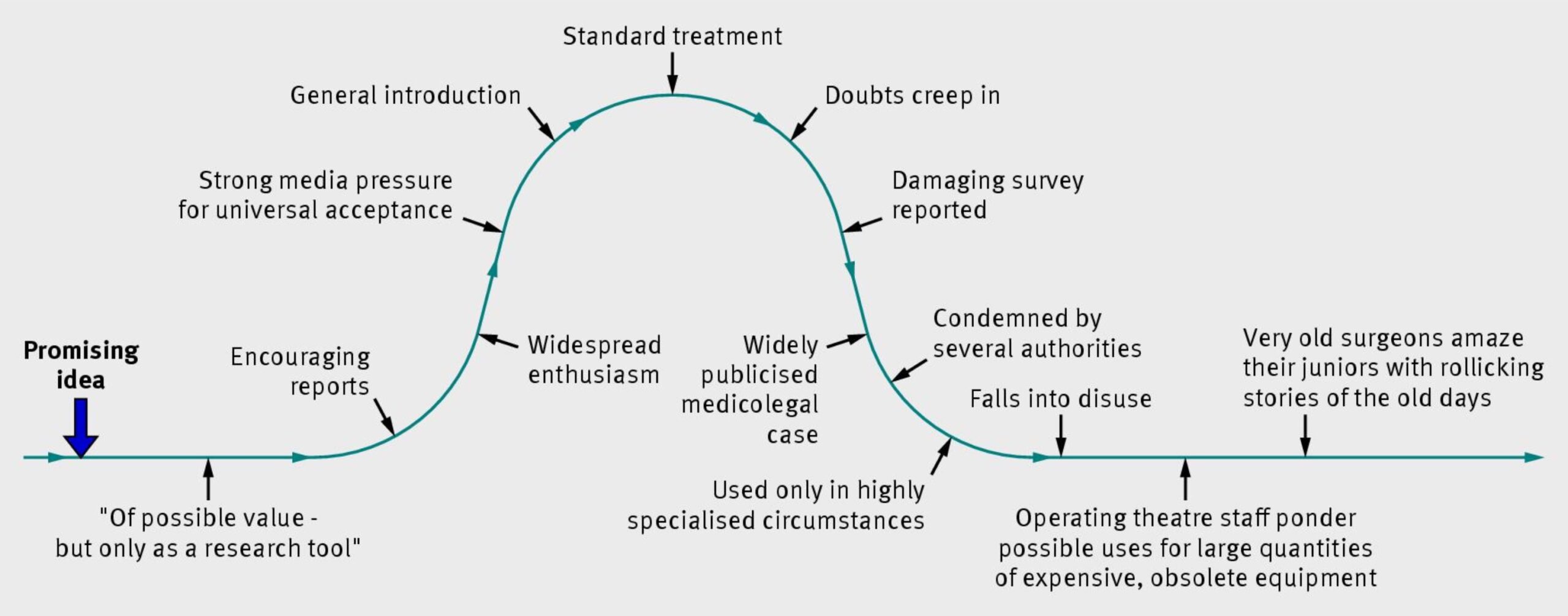
When we first saw Scott’s parabola, we had to laugh. As satire, Scott’s graphic was effective: It was the kind of deliberate exaggeration—a caricature—that could be funny while also suggesting the possibility of a serious critique. Although it was uncomfortable for us to acknowledge—especially for those of us who were orthopaedic surgeons ourselves—intuitively, we felt Scott’s joke had some truth to it.
As the years passed, though, and as clinical trials emerged interrogating the effectiveness of various orthopaedic procedures, we started to wonder whether Scott’s parabola had been more than just satire. An alarming number of common orthopaedic surgeries that were rapidly embraced by doctors on the basis of being “bio-plausible” and “intuitively rational” have not survived scientific scrutiny. When these procedures rapidly fell out of favor, might the overall trajectory of their use end up looking like Scott’s satirical graph? Could we prove that Scott’s parabola was, in fact, true?
Since we enjoyed the original fun of Scott’s parabola, we set out with some trepidation to answer this question. We liked the satire so much that we didn’t want to kill the joke. But in the end, giving ourselves license to kill turned out to be more apt than we realized.
Our Hunt for Parabolas
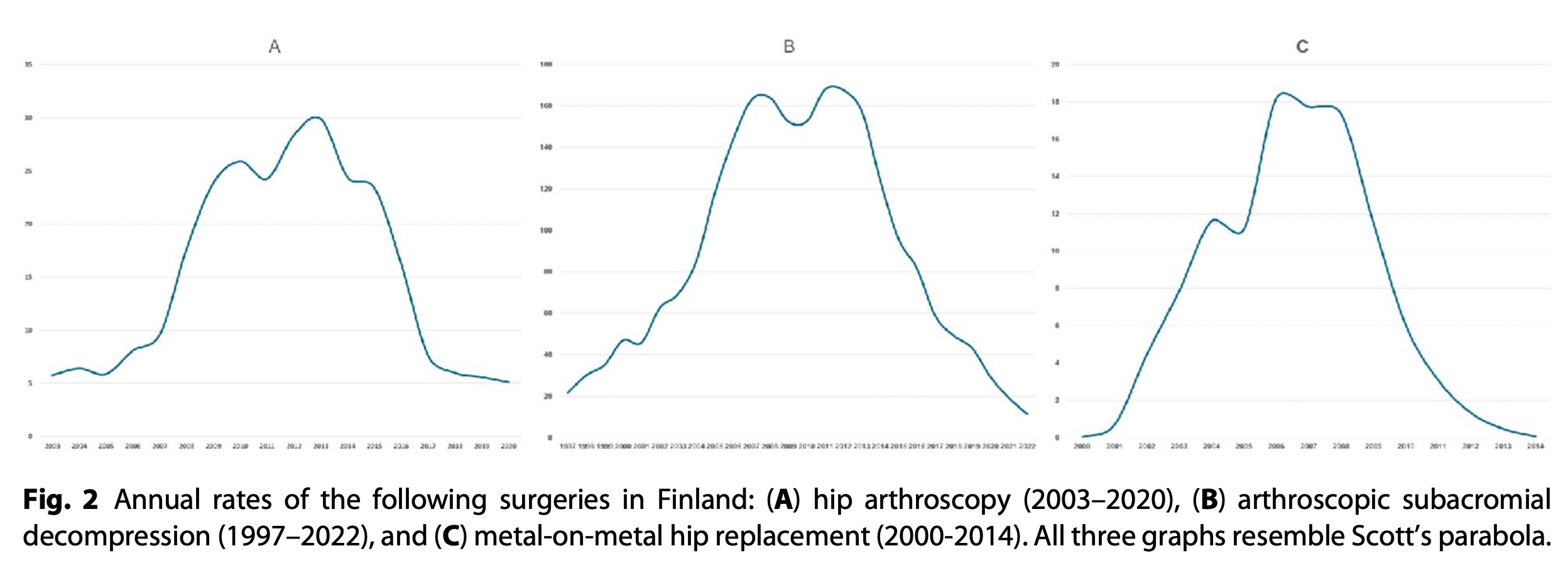
The rise and fall of three orthopaedic surgical procedures in Finland looked to us like candidates for the sort of parabolas Scott had imagined: subacromial surgeries for impingement syndrome of the shoulder, arthroscopic femoral neck osteoplasty for impingement of the hip for femoroacetabular impingement, and metal-on-metal total hip arthroplasty for hip osteoarthritis. All three of these procedures had a slow start in the late 20th century. With the arrival of arthroscopic techniques for hip and shoulder impingement early this century, the use of these procedures increased dramatically, making them some of the most common orthopaedic procedures in the world. But then major clinical trials revealed hip and shoulder arthroscopy to be ineffective for these indications. The demise was especially fast and clear in Finland—probably because Finns were involved in some of the pivotal studies. Meanwhile, with metal-on-metal arthroplasty, safety concerns soon caused a fall from grace.
With these three procedures as our test cases, we assembled their annual rates of use in the Finnish healthcare system and graphed out the results. The graphs were so reminiscent of parabolas that they made Scott look rather prophetic.
Two decades after Scott published his satirical parabola in the BMJ, we found ourselves wanting to thank him for putting us on the hunt for real parabolas. We also wanted to show him the three cases we had found that had vindicated his hunch. So, we tracked him down. Only then did we learn where Scott came up with the idea for the parabola in the first place.
Of Dalliances and Doctors
On the southern coast of England sits the town of Poole, where Scott worked as a consultant in obstetrics and gynecology at the town hospital in the 1980s. Local attractions include the chalky cliffs and beaches along the English Channel, but these are not Poole’s only claims to fame. Nearby is the former lavish estate of the family of John Bond, an Elizabethan spy whom local historians believe may have inspired aspects of the fictional secret agent, James Bond. As it turns out, Bond’s inventor, author Ian Fleming, had attended boarding school in the neighborhood.
Scott had dabbled in the local James Bond lore by reading Fleming’s 007 spy novels. While he found the cocky humor of Fleming’s secret agent funny, Scott was also an advocate for women’s health and lamented the sorry pattern of Bond’s affairs with women. This pattern was already clear in the first Bond novel Fleming had written in 1953, Casino Royale:
[Bond] found something grisly in the inevitability of the pattern of each affair…sentiment, the touch of the hand, the kiss, the passionate kiss, the feel of the body, the climax in bed, then more bed, then less bed, then the boredom, the tears and the final bitterness …
This depressing pattern was—as Fleming put into words, in Bond’s head—nothing more than a “conventional parabola”.
When we heard that Scott had seen fit to transfer the shape of a parabola from the romantic escapades of the world’s most-famous secret agent directly onto our doctorly dalliances with attractive medical techniques, we laughed again. Scott’s original satire suddenly seemed more mischievous, and funnier.
On the surface, of course, comparing the love life of a make-believe secret agent to real-world trends in medicine is ridiculous. Nevertheless, it got us thinking. After all, the purpose of even the most superficial fiction is still to hold up a mirror to the foibles and redemptions of real life.
What We Can Learn From the Hero’s Journey
The Bond in Ian Fleming’s novels was both a comic and tragic character. He was witty and seductive, but had a dark side—the merciless license to kill and his failure to find true love. This tragicomic tension at the heart of his character remained part of Bond’s appeal. But Bond’s character also evolved over the years, first from the pages of Fleming’s novels into film adaptations, then into a series of new screenplays, as well as through the different actors who portrayed Bond on the silver screen.
The first actor, Sean Connery, amplified Bond’s comic side, starting with the first Bond film in 1962, Dr. No. In Connery’s view, more humor would make Bond’s violations of decorum more benign and his overall character more acceptable—perhaps a bit like the satire in the original Scott’s parabola.
This “tongue-in-cheek” Bond had a long and successful run. But Bond’s frivolous affairs and quips became passé. By the 21st century, when actor Daniel Craig strode into the role, his world had become more evidently corrupted and complicated. Bond had to tip farther into his tragic side to find meaning, facing his flaws and mistakes. Only then could the character—and the jokes—continue to resonate. This transformation has been riveting to watch. Bond on screen—spoiler alert—grew more humble and vulnerable, evolving from promiscuity to fealty to, in the last film, fatherhood.
We can’t help seeing the parallels to our own profession. We surgeons have had a long run too, championing evermore technical procedures that arrive with a glamorous shine. Often, we are kitted out as if we’d just come from a meeting with Q, 007’s procurer of gadgets—indeed, our device manufacturers play a similar role. When an attractive new surgical technique comes along, this can make it hard to say “no”.
Yet if we want to retain credibility with our “audience” of patients for the long haul, we should take inspiration from the later, more-human Bond. After all, if even the notorious James Bond can reform himself, then surely we can, too. For starters, we could develop more humility—we err as individuals, and the patterns we’re discussing here suggest that we err systemically, too. Scott’s Bond-inspired parabola has turned out to be truer than we realized, at least for some orthopaedic procedures. If we keep falling into frivolous affairs, our claims to expertise will become less convincing, and patients may stop trusting us.
Two things we could do better would be to bring greater skepticism and scientific scrutiny to new techniques before we adopt them and to conduct more, better-quality trials to test the effectiveness of current practices. For hip and shoulder arthroscopy, it was rigorous scientific trials that discovered problems and initiated the down slope of the parabola. No doubt, more of these parabolas could be mapped.
We also suspect that medicine may be inundated with “half parabolas”—procedures that have shot up in popularity but have not yet been scrutinized and brought back down. Many techniques are persuasively marketed, but far fewer have been subjected to the same rigorous study as hip and shoulder arthroscopies. And unfortunately, even when such tests have been conducted, we clinicians often aren’t informed or convinced in sufficient numbers to end the romance. It’s been suggested that in the United States, at least one-third of all current medical expenditures are ineffective or unnecessary, but that has not stopped the waste. In fact, the problem may not only be James Bond–style affairs, but a rash of plateaued marriages that could precipitate a messy epidemic of divorce without proactive intervention. The more we can implement rigorous trials to test the effectiveness of our current techniques, the better chance we have at identifying best practices while also managing the down slope when procedures turn out to be flawed or ineffective. In turn, we will know better how to test new procedures before we let ourselves fall in love with them in the first place.
A mature surgical profession will be able to stop these parabolic affairs before they start. In time, we might even pull off a satisfying punchline: bringing the phenomenon of the parabolic rise and fall of problematic medical techniques itself to a parabolic end. The results would include fewer risks, lower costs, and better patient health. Unlike James Bond, surgeons should not be tragicomic characters, but characters who inspire trust.❦